Each year, World Thrombosis Day (October 13) provides an opportunity for Thrombosis Canada to raise awareness about thrombosis (blood clots), the risk factors and warning signs, prevention measures, and treatment.

While it may seem cliché, knowledge is power and while we’re often educated on the warning signs for a stroke or heart attack, venous thrombosis or blood clots in the leg or in the lungs can be a serious and even life-threatening medical condition. Here’s what you need to know about venous blood clots, signs and symptoms, risk factors and how to manage them with your healthcare team:
What is a Deep Vein Thrombosis (DVT)?
A deep vein thrombosis (DVT) is a blood clot that forms in one of the deep veins in the body, typically in the legs. When a DVT occurs blood cells accumulate abnormally and form a clot within a vein. As a result of the clot, there can be pain, swelling and redness, usually in only one leg. Treatment for a DVT involves using anticoagulant medications (commonly referred to as blood thinners). These prevent the clot from growing larger and reduce the risk of it breaking free and travelling to the lungs causing a pulmonary embolism (PE).

What is a Pulmonary Embolism (PE)?
A DVT can lead to a more serious medical condition if a clot breaks free from the vein and travels to the lungs causing a potentially life-threatening condition called pulmonary embolism (PE). A PE is when a blood clot lodges itself in one or more of the arteries of the lungs stopping blood flow to part of the lung which can lead to serious complications. Prompt treatment greatly reduces the risk of serious and life-threatening complications.

What are the Risk Factors for developing a Venous Blood Clot?
About one out of every 1,000 adults develop DVT and/or PE each year. Some of the most common major risk factors are:
- Surgery – major surgeries increase the risk of blood clots especially orthopedic surgery, vascular surgery, neurosurgery, and cancer surgery
- Cancer – people living with or undergoing treatment for cancer have a high risk of blood clots
- Hospitalization for acute medical illness – the risk increases during hospitalization and most events happen six to 12 weeks after hospital discharge
- Fractures/trauma – all kinds of major trauma increase the risk of blood clots
- Age – the incidence of blood clots increases with age, especially for people over 60
- Obesity – being overweight increases the risk of developing a blood clot
- History of blood clots – people with a previous blood clot, especially unexplained blood clots, are at higher risk to develop them again
- Family history – the risk of developing blood clots is higher in people with one or more first-degree family members (parent, sibling, child) who had blood clots, especially when the blood clot was unexplained, occurred at a young age, and affected multiple family members even when testing for inherited clotting abnormalities is normal
- Pregnancy – the risk of blood clots is increased during pregnancy and in the postpartum period
- Estrogen-containing hormone therapy can also increase the risk for some women.
What are the Signs or Symptoms of a Blood Clot?
Seek medical attention if you have any signs or symptoms of a DVT or PE. Use the acronym CLOTS to keep the key signs and symptoms in mind:
Chest Pain – a blood clot in the lung can cause local damage, resulting in sharp chest pain
Light-Headedness – a blood clot in the lung causes light-headedness or dizziness and can even cause people to faint
Out of Breath – a blood clot in the lung makes it harder for blood to get oxygen from the lungs causing difficulty breathing
Leg Tenderness – a blood clot in the leg causes tenderness or cramping in the calf or behind the knee, as well as redness and warmth
Leg Swelling – A blood clot in the leg blocks blood flow to the veins that drain blood from the leg back to the heart. This causes the leg to swell.
How do you Treat or Prevent a Blood Clot?
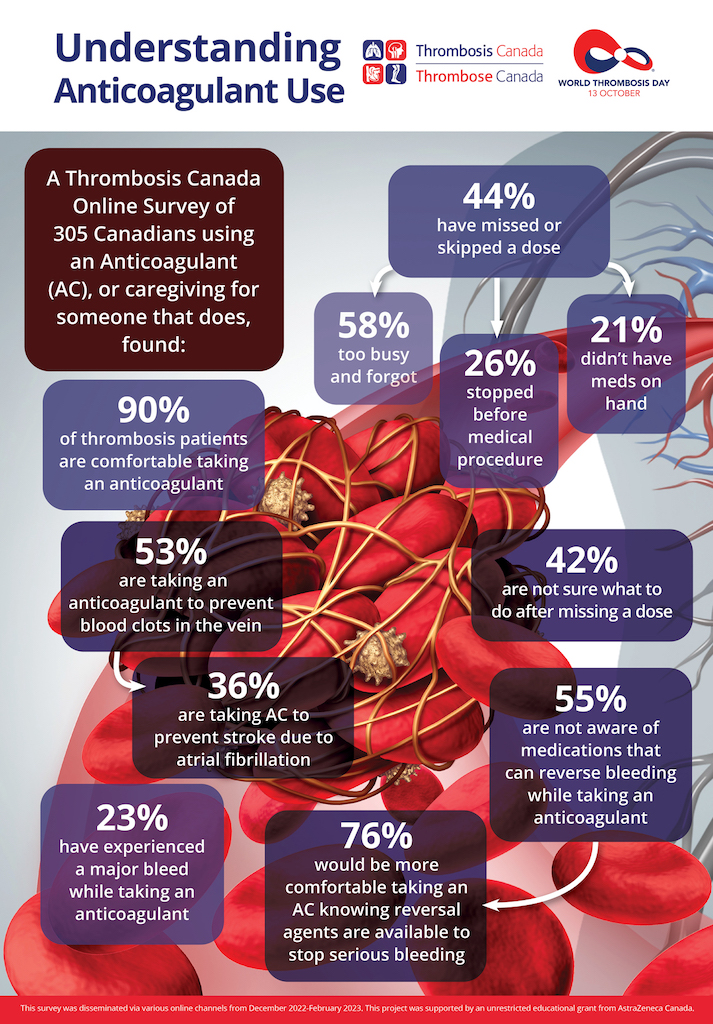
- Anticoagulants (sometimes referred to as blood thinners are) widely used to treat or prevent blood clotting
- Some conditions treated with anticoagulants include:
- Atrial fibrillation – an abnormal heart rhythm that increases the chances of stroke or blood clot that travels to the brain
- Venous thrombosis – pulmonary embolism and/or deep vein thrombosis
- Mechanical heart valve
- Anticoagulants work by interfering with the blood clotting process and reduce the risk of existing blood clots growing larger and preventing new blood clots from forming
What are the Side Effects of Anticoagulants?
- Anticoagulants increase the chances of bleeding – they do not cause bleeding but can make it worse as they interfere with blood clotting which normally helps to stop the bleed
- When major (serious) bleeding occurs while taking an anticoagulant, urgent care is often required in an emergency department or hospital
- When non-major (less serious) bleeding occurs, it does not last long and stops on its own requiring no medical assistance. It is important to let your healthcare provider know about bleeding while on anticoagulants.
There are treatments that can be used to counteract or reverse the effect of anticoagulants to help stop serious bleeding emergencies.
Have more questions about thrombosis? Visit thrombosiscanada.ca for more information including patient fact sheets and videos about thrombosis, its treatment and management.

Dr. Deborah Siegal is an Associate Professor in the Department of Medicine within the Division of Hematology at the University of Ottawa, and Scientist in the Clinical Epidemiology Program at the Ottawa Hospital Research Institute. She is on the Leadership Team at Thrombosis Canada.