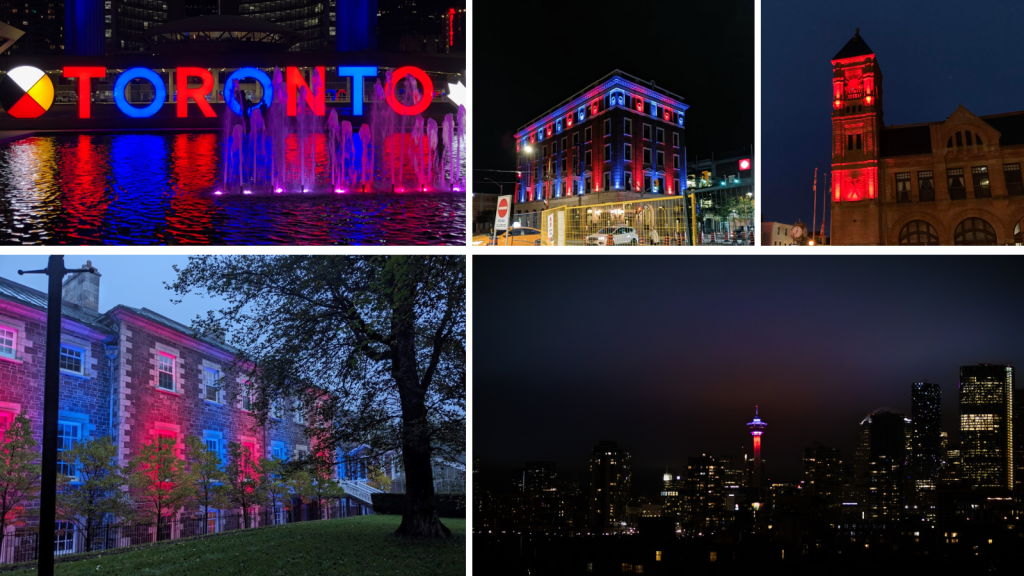
Each year, Thrombosis Month (October) provides an opportunity for Thrombosis Canada to share facts about venous thrombosis (blood clots) and raise awareness about it; the risk factors and warning signs, prevention measures, and treatment.
As a 36-year-old thrombosis survivor, I learned the hard way that you don’t know what you don’t know. After my thrombosis journey, I’m committed to sharing my story so that people can recognize the signs and symptoms of thrombosis, know the risk factors and how to prevent them and most importantly, be aware that serious, life-threatening blood clots can happen to anyone at any time. Take my word, it’s not a condition that can occur only in older adults.
Here’s my story …
Back in the summer of 2019, I was recovering from a surgery following a car accident. In November of 2017, I was hit by a car as a pedestrian, which broke my pelvis and ribs in multiple places. Almost two years after the incident, I was still dealing with complications from the injury, and had surgery to repair a tear in the cartilage of my left hip. Around three weeks later, my boyfriend, Ryan (now husband) was helping me with physiotherapy exercises in the basement of our house. In the days leading up to my thrombosis event, I had noticed some swelling in my leg as well as some shortness of breath, but I brushed it off as a side effect of my recent surgery along with my subsequent inactivity.

The nausea hit without a warning. Seconds later, I started having what Ryan described as a string of severe seizures. I kept phasing in and out of consciousness, and whenever I came to, I felt like I couldn’t breathe.
Ryan was alarmed and quickly called 911. Paramedics showed up within minutes and prepared to take me to the hospital. Initially, I was unresponsive but would occasionally wake up briefly and slip back into unconsciousness. Once in the ambulance, they lost my vital signs and immediately began to perform CPR. While they initially were unable to stabilize me, the determined team continued tirelessly, and signs of life finally returned. Moments later, my vital signs were lost again, and the team repeated the CPR to stabilize me and get me to the hospital.
The last thing I remember is being wheeled out of my garage on a stretcher, struggling to breathe. I remember saying “I’m sorry, Ryan. I love you.” The next thing I knew, it was a day later and I was in a hospital bed in the ICU completely disoriented. I didn’t know where I was, what had happened, or why there were so many tubes sticking out of my body.

Doctors soon explained I had experienced a deep vein thrombosis (DVT). A clot had formed in my leg, then broke loose and made its way to my lungs, causing a pulmonary embolism (PE) so severe that I endured multiple cardiac arrests. I was effectively dead for about thirty minutes in total. Even the doctors at the hospital believe that it was thanks to a series of miracles that I’m alive today.

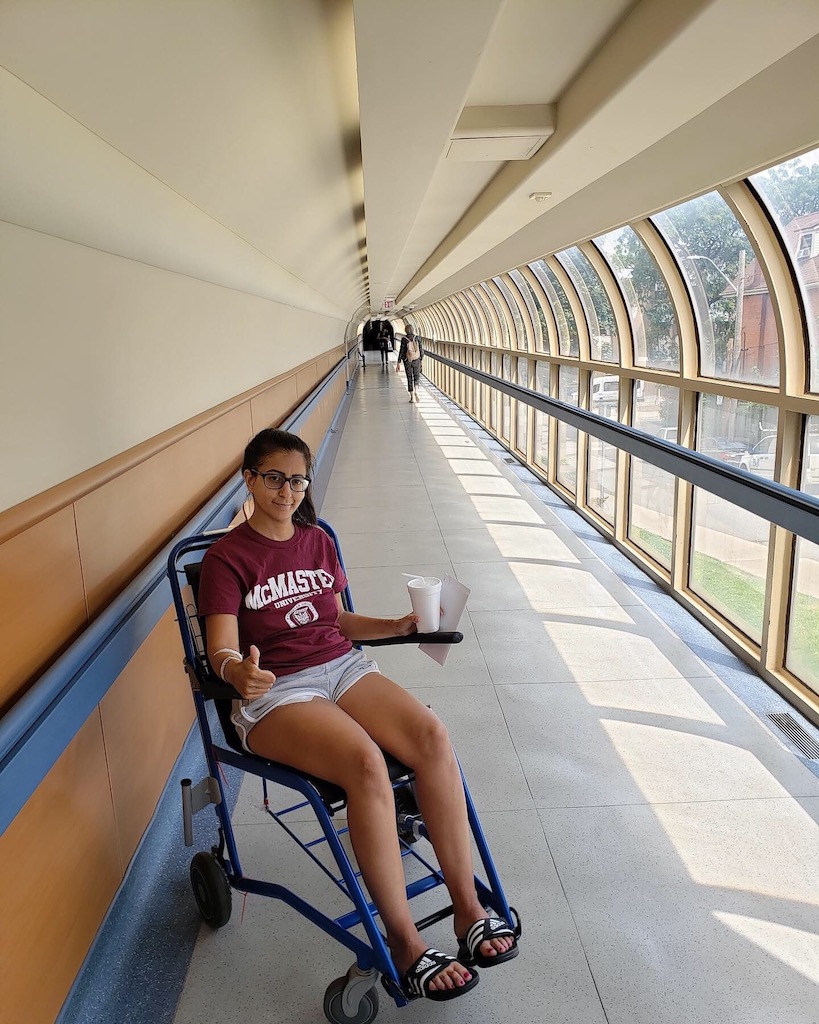
All of this happened several years ago, but I’ll never forget the top-notch services and treatments I received. Between the paramedics who performed textbook CPR and the staff at St. Joseph’s Healthcare Hamilton who diagnosed and treated me, I will forever be grateful for the efforts that were made to save my life during the scariest 24 hours my family has ever experienced. I have since made a full recovery, and now take blood thinners daily to prevent further episodes.
Through my own research, I have discovered that PEs are not unheard of in women of my age, especially among women who take an oral contraceptive or have had recent C-sections. People who are close to me are now very aware of the risks and symptoms, and I want that knowledge to reach as far and wide as possible. No one thinks it could happen to someone in their early thirties – and yet, it does.
I have been very open about my story on social media, and I now regularly receive questions about my experience as well as words of appreciation for sharing it so widely.

I would like to see more research going into what causes incidents like I experienced. Despite his expertise, my doctor was completely stumped as to what caused my experience to be one that was so severe. They ran genetic tests and nothing conclusive came up, but I’m hopeful that further research will uncover the exact cause of the event.
I have always been passionate about giving back to my community, having volunteered with my school for many years and at the hospital where I was treated for my blood clot. I jumped at the opportunity to work with Thrombosis Canada to help people learn more about blood clots and know what to do if they ever had a similar experience to mine. I encourage you to take a minute and learn the basics about blood clots.
THE FACTS ABOUT VENOUS THROMBOSIS
What is a DVT?
A deep vein thrombosis (DVT) is a blood clot that forms in one of the deep veins in the body, typically in the legs. When a DVT occurs blood cells accumulate abnormally and form a clot within a vein. As a result of the clot, there can be pain, swelling and redness, usually in only one leg. Treatment for a DVT involves using anticoagulant medications (commonly referred to as blood thinners). These prevent the clot from growing larger and reduce the risk of it breaking free and travelling to the lungs causing a pulmonary embolism (PE).
What is a PE?
A DVT can lead to a more serious medical condition if a clot breaks free from the vein and travels to the lungs causing a potentially life-threatening condition called pulmonary embolism (PE). A PE is when a blood clot lodges itself in one or more of the arteries of the lungs stopping blood flow to part of the lung which can lead to serious complications. Prompt treatment greatly reduces the risk of serious and life-threatening complications.
What are the risk factors for developing a venous blood clot?
About one out of every 1,000 adults develop DVT and/or PE each year. Some of the most common major risk factors are:
- Surgery – major surgeries increase the risk of blood clots especially orthopedic surgery, vascular surgery, neurosurgery, and cancer surgery
- Cancer – people living with or undergoing treatment for cancer have a high risk of blood clots
- Hospitalization for acute medical illness – the risk increases during hospitalization and most events happen six to 12 weeks after hospital discharge
- Fractures/trauma – all kinds of major trauma increase the risk of blood clots
- Age – the incidence of blood clots increases with age, especially for people over 60
- Obesity – being overweight increases the risk of developing a blood clot
- History of blood clots – people with a previous blood clot, especially unexplained blood clots, are at higher risk to develop them again
- Family history – the risk of developing blood clots is higher in people with one or more first-degree family members (parent, sibling, child) who had blood clots, especially when the blood clot was unexplained, occurred at a young age, and affected multiple family members even when testing for inherited clotting abnormalities is normal
- Pregnancy – the risk of blood clots is increased during pregnancy and in the postpartum period
- Estrogen-containing hormone therapy can also increase the risk for some women.
What are the signs or symptoms of a blood clot?
Seek medical attention if you have any signs or symptoms of a DVT or PE. Use the acronym CLOTS to keep the key signs and symptoms in mind:
Chest Pain – a blood clot in the lung can cause local damage, resulting in sharp chest pain
Light-Headedness – a blood clot in the lung causes light-headedness or dizziness and can even cause people to faint
Out of Breath – a blood clot in the lung makes it harder for blood to get oxygen from the lungs causing difficulty breathing
Leg Tenderness – a blood clot in the leg causes tenderness or cramping in the calf or behind the knee, as well as redness and warmth
Leg Swelling – A blood clot in the leg blocks blood flow to the veins that drain blood from the leg back to the heart. This causes the leg to swell.

How do you treat or prevent a blood clot?
- Anticoagulants (sometimes referred to as blood thinners are) widely used to treat or prevent blood clotting
- Some conditions treated with anticoagulants include:
- Atrial fibrillation – an abnormal heart rhythm that increases the chances of stroke or blood clot that travels to the brain
- Venous thrombosis – pulmonary embolism and/or deep vein thrombosis
- Mechanical heart valve
- Anticoagulants work by interfering with the blood clotting process and reduce the risk of existing blood clots growing larger and preventing new blood clots from forming
What are the side effects of anticoagulants?
- Anticoagulants increase the chances of bleeding – they do not cause bleeding but can make it worse as they interfere with blood clotting which normally helps to stop the bleed
- When major (serious) bleeding occurs while taking an anticoagulant, urgent care is often required in an emergency department or hospital
- When non-major (less serious) bleeding occurs, it does not last long and stops on its own requiring no medical assistance. It is important to let your healthcare provider know about bleeding while on anticoagulants.
- There are treatments that can be used to counteract or reverse the effect of anticoagulants to help stop serious bleeding emergencies.
Have more questions about thrombosis? Visit thrombosiscanada.ca for more information including patient fact sheets and videos about thrombosis, its treatment and management.
